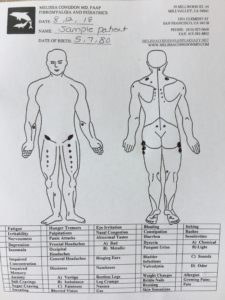
Does this sound like an outlandish claim? It is not. I was diagnosed with fibromyalgia 10 years ago by fibromyalgia expert Dr. R. Paul St. Amand. He uses a method of palpation which he calls “body mapping,” where he carefully uses his finger pads to find any swollen areas of muscles, tendons, and ligaments in the body, and records his findings on a “body map.” These areas need not be tender (super important because when the tender point exam was evaluated in 2010 it was found to be inaccurate — missing over 20% of people with known fibromyalgia — plus the tender point exam does not take into account any of the non-pain symptoms of fibromyalgia, such as non restorative sleep, possible fatigue, headaches, dizziness, etc. Turns out the tender point exam was never meant to be used in a clinical setting anyway, it was meant to be a research tool). Dr. St. Amand has found that 100% of people with fibromyalgia have swollen areas of muscles, tendons, and ligaments in their left anterior thigh (these swollen areas are usually very small and don’t often hurt, so most people with fibromyalgia aren’t aware of their presence). I trained with Dr. St. Amand to learn how to do the mapping exam.
So why is this important? Firstly, it allows me to quickly and accurately diagnose fibromyalgia during the first office visit. The other available options (other than the tender point exam) are the American College of Rheumatology 2010 criteria–but that requires physicians to “interview patients and determine the severity of fatigue, sleep, and cognitive problems, and the overall degree of somatic symptom reporting. It seems certain that physicians will differ in their conscientiousness in making such assessments and their interpretation of the severity of patient complaints,” https://onlinelibrary.wiley.com/doi/full/10.1002/art.38908, and the FM/a blood test may be 94% accurate, but may not be covered by insurance (it retails for $936) and some physicians question whether people with Lyme disease (or other conditions) may test erroneously test positive for fibromyalgia. For the cost of an office visit, my patients get an accurate diagnosis and a personalized treatment plan.
Secondly it allows me to identify people who have been misdiagnosed with fibromyalgia. If I see someone in my office for a fibromyalgia evaluation and they do not have anterior thigh nodules they DO NOT HAVE FIBROMYALGIA. Later, these patients were accurately diagnosed with conditions such as celiac disease, Ehlers-Danlos or other connective tissue disease, Lyme disease, actively replicating virus in their system (such as EBV) which gave them symptoms of chronic widespread pain.
I am so thankful to Dr. St. Amand for teaching me how to do the mapping exam. He and I have trained/continue to train healthcare professionals how to map. Wouldn’t it be wonderful if more healthcare professionals were interested in learning how to map? Then they could accurately and quickly diagnose fibromyalgia (for the cost of an office visit) and understand that the physical exam in people with fibromyalgia is NOT NORMAL, but has a collection of swollen muscles, tendons, and ligaments. Even more proof that fibromyalgia is a real syndrome.